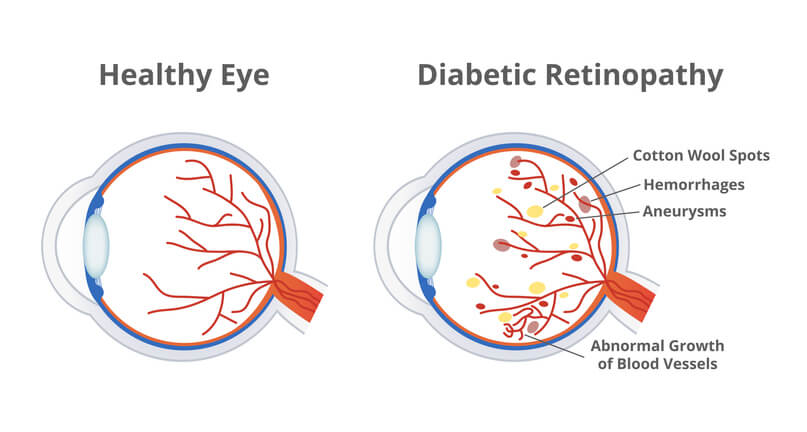
Diabetic retinopathy is a complication of diabetes that affects the eyes. This eye disease occurs when high blood sugar levels damage the tiny blood vessels in the retina. The retina is the light-sensitive tissue at the back of the eye.
Over time, these damaged blood vessels can leak fluid and cause blurred vision. It can even cause new abnormal blood vessels to grow on the surface of the retina. Diabetic retinopathy is one of the leading causes of blindness among working-age adults.
Treatment for diabetic retinopathy depends on how far it has progressed. Intravitreal injections and other forms of treatment may be necessary to preserve and restore vision. Laser surgery may also be able to seal off leaking blood vessels and stop further damage from occurring.
There are various drugs that can be used to treat diabetic retinopathy. Examples of these drugs include steroids, which help reduce inflammation, and Anti-VEGF agents which can decrease swelling and prevent new abnormal blood vessel formation.
In addition to drug treatments, laser surgery is also commonly used to treat complications of diabetic retinopathy and stop further damage from occurring.
Diabetic retinopathy is caused by prolonged exposure to high blood sugar levels. People who have diabetes and fail to manage their condition properly are at greater risk of developing diabetic retinopathy. Additionally, people with high cholesterol, high blood pressure, heart disease or a family history of diabetes are also more likely to experience diabetic retinopathy.
Diabetic Retinopathy SymptomsDiabetic retinopathy typically has no symptoms in the early stages. This makes it difficult to detect. As it progresses, common symptoms of diabetic retinopathy include blurry vision and darkened areas in your field of vision where parts of your vision are missing.
If you experience any of these symptoms, it’s important to contact a doctor immediately so that they can assess the severity of your condition and provide appropriate treatment.
Our SpecialistDiagnosis starts with a comprehensive eye exam. If a doctor suspects diabetic retinopathy, he will use imaging tests such as an optical coherence tomography (OCT) scan, fluorescein angiography (FA), or optical coherence tomography angiography (OCT-A) to evaluate the condition of the retina and detect any abnormal blood vessels.
The best way to prevent diabetic retinopathy is by managing diabetes properly. This includes monitoring your blood sugar levels. Following a healthy lifestyle with regular exercise and balanced nutrition also helps.
Additionally, you should visit your doctor regularly for comprehensive eye exams to check for signs of diabetic retinopathy. Regular eye exams will detect changes or complications with the retina and ensure prompt treatment if necessary.
Diabetic retinopathy is a serious complication of diabetes that can lead to blindness if left untreated. It is important to manage your diabetes properly and have regular check-ups with an eye doctor to reduce the risk of developing diabetic retinopathy. With proper treatment, it is possible to reduce vision loss and preserve sight.
Our retina specialists are the Lehigh Valley’s premier choice for diagnosing and treating diabetic retinopathy. If your doctor has referred you to Lehigh Eye Specialists, know that you will receive the utmost attention from our highly skilled doctors and compassionate staff. We welcome you to learn more about our practice and meet our doctors and staff. Our Patient Portal page will provide you with information and forms to help you prepare for your appointment.
About Lehigh Eye Specialists Patient Resources